Pertaining To Destruction Of Worn-out Red Blood Cells
listenit
Mar 30, 2025 · 7 min read
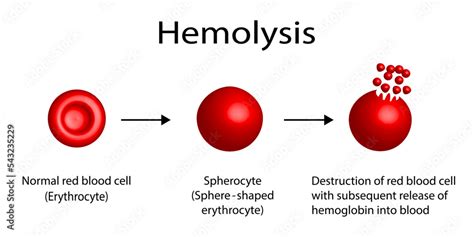
Table of Contents
The Demise of Worn-Out Red Blood Cells: A Journey Through Erythrokinetic Destruction
Red blood cells (RBCs), also known as erythrocytes, are the tireless workhorses of our circulatory system. These tiny, biconcave discs tirelessly ferry oxygen from our lungs to every corner of our bodies, a crucial process for sustaining life. But like all cellular components, RBCs have a limited lifespan, typically around 120 days. Understanding the intricate mechanisms that govern their destruction, a process known as erythrokinetic destruction, is vital for comprehending overall health and diagnosing various hematological disorders. This article delves deep into the fascinating world of worn-out red blood cell destruction, exploring its various pathways and the crucial roles played by the spleen, liver, and bone marrow.
The Aging Process: Why Red Blood Cells Wear Out
The lifespan of an RBC is dictated by several factors, primarily its inherent vulnerability to oxidative stress and the gradual loss of its crucial structural integrity. As RBCs age, they accumulate damage from various sources:
Oxidative Stress: The Silent Assassin
Oxygen, the very substance RBCs transport, is a double-edged sword. While essential for life, oxygen metabolism generates reactive oxygen species (ROS), highly reactive molecules that inflict damage on cellular components. This oxidative stress leads to lipid peroxidation in the RBC membrane, compromising its flexibility and deformability. The resulting stiffening makes it difficult for aged RBCs to navigate the narrow capillaries, leading to their eventual destruction.
Membrane Damage and Protein Degradation
The RBC membrane, a complex structure of proteins and lipids, is crucial for maintaining its shape and flexibility. Over time, this membrane undergoes progressive damage. Proteins within the membrane, like spectrin and ankyrin, essential for maintaining its structural integrity, become degraded. This degradation further contributes to the loss of membrane flexibility, making the cells more susceptible to destruction.
Loss of Enzymes and Metabolic Function
RBCs rely on specific enzymes for vital metabolic functions. As they age, the activity of these enzymes decreases, impairing their ability to maintain cellular homeostasis. This compromised metabolism further contributes to the accumulation of cellular damage, accelerating the aging process.
The Sites of Destruction: A Coordinated Effort
The demise of worn-out RBCs isn't a haphazard event. The body employs a sophisticated system, primarily involving the spleen, liver, and bone marrow, to efficiently remove these aging cells and recycle their valuable components.
The Spleen: The RBC Graveyard
The spleen, often dubbed the "red blood cell graveyard," plays a pivotal role in removing senescent RBCs from circulation. Its unique structure, with its dense network of splenic cords and narrow sinusoids, acts as a filter. As RBCs navigate these tight spaces, those with compromised membrane flexibility and deformability are unable to pass through, becoming trapped and subsequently destroyed. This process, termed extravascular hemolysis, is the primary mechanism for the removal of aged RBCs. The spleen's macrophages, specialized phagocytic cells, engulf and break down the trapped RBCs, releasing hemoglobin for recycling.
The Liver: A Secondary Site of Destruction
While the spleen is the main site of RBC destruction, the liver also contributes to this process. The liver's Kupffer cells, another type of macrophage, can phagocytose senescent RBCs, though to a lesser extent than the spleen. This process also contributes to extravascular hemolysis. The liver plays a significant role in processing the hemoglobin released during RBC breakdown, further contributing to heme catabolism.
The Bone Marrow: A Balancing Act
The bone marrow, responsible for producing new RBCs, also plays a less prominent role in their destruction. Intramedullary hemolysis, the destruction of RBCs within the bone marrow, occurs at a much lower rate compared to extravascular hemolysis in the spleen and liver. However, it becomes more significant in certain conditions characterized by increased RBC destruction, such as hemolytic anemias.
Hemoglobin Recycling: A Symphony of Biochemical Processes
The destruction of RBCs isn't simply a disposal process; it's a tightly regulated biochemical pathway aimed at recovering and recycling valuable components. The most critical aspect of this recycling is the processing of hemoglobin, the oxygen-carrying protein within RBCs.
Heme Catabolism: From Heme to Bilirubin
Hemoglobin is broken down into its constituent parts: heme, globin, and iron. Heme, the iron-containing porphyrin ring, undergoes a series of enzymatic reactions, ultimately leading to the formation of bilirubin, a yellowish pigment. This process, termed heme catabolism, involves several key enzymes, including heme oxygenase, which converts heme to biliverdin. Biliverdin is then reduced to bilirubin, which is transported to the liver bound to albumin.
Globin Degradation: Recycling Amino Acids
The globin portion of hemoglobin, a protein composed of amino acids, is further broken down into its constituent amino acids. These amino acids are then released into the bloodstream and reused by the body for protein synthesis. This recycling process is crucial for maintaining the body's amino acid pool.
Iron Recycling: A Precious Commodity
Iron, a crucial component of heme, is also meticulously recycled. Iron released during hemoglobin breakdown is transported bound to transferrin, a plasma protein, to the bone marrow. Here, it is incorporated into new heme molecules during erythropoiesis, the process of RBC production. This efficient iron recycling minimizes the body's need for dietary iron intake.
Consequences of Impaired Erythrokinetic Destruction: Hemolytic Anemias
Dysfunction in the normal process of RBC destruction can lead to a variety of hematological disorders, most notably hemolytic anemias. These conditions are characterized by an accelerated rate of RBC destruction, exceeding the bone marrow's capacity to compensate. This imbalance leads to anemia, a deficiency of red blood cells or hemoglobin.
Types of Hemolytic Anemias
Hemolytic anemias can be broadly classified into inherited and acquired forms. Inherited hemolytic anemias, like sickle cell anemia and thalassemia, result from genetic defects affecting the structure or function of RBCs, rendering them more susceptible to premature destruction. Acquired hemolytic anemias can result from various factors, including autoimmune diseases, infections, and exposure to certain drugs or toxins.
Symptoms and Diagnosis
The symptoms of hemolytic anemia often reflect the severity of RBC destruction and the body's ability to compensate. These symptoms can range from mild fatigue and pallor to jaundice (yellowing of the skin and eyes) and splenomegaly (enlarged spleen). Diagnosis typically involves blood tests to evaluate RBC count, hemoglobin levels, and reticulocyte count (immature RBCs). Further investigations, such as bone marrow examination and genetic testing, may be necessary to identify the underlying cause of hemolysis.
Therapeutic Interventions: Managing Hemolytic Anemias
Treatment for hemolytic anemia depends on the underlying cause and the severity of the condition. In some cases, supportive care, including blood transfusions and iron supplementation, may suffice. For inherited hemolytic anemias, genetic counseling and supportive therapies are crucial. In certain cases, splenectomy, the surgical removal of the spleen, might be considered to reduce the rate of RBC destruction. For autoimmune hemolytic anemias, immunosuppressant medications may be used to suppress the immune system's attack on RBCs. New avenues of research are exploring gene therapy and other targeted therapies to address the root cause of specific hemolytic anemias.
Conclusion: A Delicate Balance
The destruction of worn-out red blood cells is a finely tuned process essential for maintaining overall health. This intricate mechanism, involving the coordinated efforts of the spleen, liver, and bone marrow, ensures the efficient removal of aged RBCs and the recycling of valuable components. Understanding the complexities of erythrokinetic destruction is crucial for diagnosing and managing various hematological disorders, particularly hemolytic anemias. Continued research in this area promises to further refine our understanding of this vital biological process and pave the way for novel therapeutic interventions. The delicate balance between RBC production and destruction highlights the remarkable efficiency and precision of our bodies' self-regulating systems. This complex interplay underscores the importance of maintaining overall health and addressing any potential dysfunctions promptly. Further research into the intricacies of erythrokinetic destruction will undoubtedly unveil even more fascinating details about this fundamental biological process.
Latest Posts
Latest Posts
-
What Type Of Symmetry Do Sea Stars Have
Apr 01, 2025
-
How Many Fluid Ounces Are In A Fifth
Apr 01, 2025
-
What Is The Fraction Of 0 85
Apr 01, 2025
-
54 As A Product Of Prime Factors
Apr 01, 2025
-
How Do You Write 3 2 As A Percentage
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Pertaining To Destruction Of Worn-out Red Blood Cells . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
